Tips to prevent reject reason code C7010
You receive this reason code when the beneficiary was or is enrolled in a hospice election period for the date of service(s).
- Confirm the beneficiary’s eligibility via direct data entry (DDE) or Secure Provider Online Tool (SPOT).
- If the information is invalid:
- Contact the hospice provider and ask them to submit their last claim for the beneficiary with occurrence code 42 and the date of disenrollment. Once the records are deleted or updated, refile the claim to Medicare.
- If the information is valid and the services provided to the beneficiary are related to their terminal condition for hospice services:
- Refile the claim with the hospice provider listed on the beneficiary’s records.
- If the information is valid and the services provided to the beneficiary are not related to their terminal condition for hospice services:
- Refile the claim with a condition code 07 (treatment of non-terminal condition for hospice patient).
- If the information is invalid:
Refer to the Part A Reason Code Lookup for a description associated with the Medicare Part A reason code(s). Enter a valid reason code into the box and click the submit button.
SPOT users
- Visit the Check Eligibility page and search by date of service and beneficiary information.
- On the Eligibility / Benefits results page, select the Hospice / Home Health tab (when available).

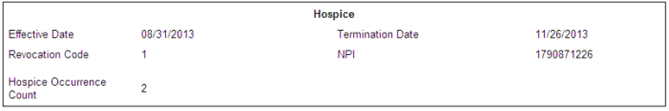
- The beneficiary’s hospice results will include the following information:
- Effective date
- Termination date
- Revocation code:
- 0 = No revocation, open spell
- 1 = Revoked by beneficiary
- 2 = Revoked (occurrence code 42)
- 3 = Revoked (occurrence code 23)
- NPI
- Search the NPI registry for the hospice provider’s contact information
- Hospice occurrence count (when applicable)
Reference