COVID-19 vaccine and monoclonal antibody billing for Part B providers
This article will assist Medicare Part B providers with proper billing relating to Coronavirus (COVID-19) vaccine and monoclonal antibody (mAb) infusion. Beneficiary coinsurance and deductible are waived.
How to bill for COVID-19 vaccines and monoclonal antibodies
For billing single claims for COVID-19 vaccines and monoclonal antibodies, follow the instructions below.
- For roster billing and centralized billing refer to the Medicare billing for COVID-19 vaccine shot administration page.
- Effective for dates of services on and after January 1, 2022, COVID-19 vaccines and mAbs provided to patients enrolled in a Medicare Advantage plan are to be billed to the Medicare Advantage plan.
For coding, effective dates and payment allowances for COVID-19 vaccines, refer to the CMS vaccine pricing – COVID-19 vaccines and monoclonal antibodies.
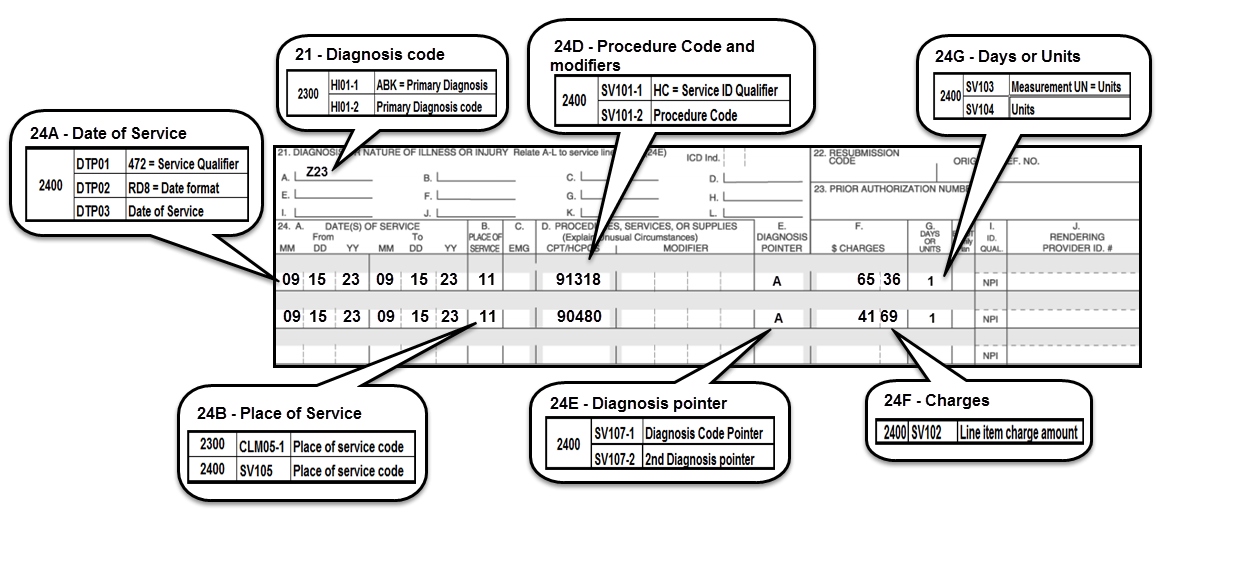
Claim submission example:
- Claim should include the proper billing of the ICD-10, Z23, in item 21 or the EDI equivalent:
- Report the proper date of service
- Report the proper place of service
- Use the applicable CPT or HCPCs code
- The diagnosis pointer should be used to indicate the primary diagnosis on the claim form
- Report the charge amount for each line item
HCPCS M0201 (administration of pneumococcal, influenza, hepatitis b, and/or covid-19 vaccine inside a patient's home) can be billed if it meets the criteria outlined in the following CMS resources:
- Medicare payment for COVID-19 vaccination administration in the home
- Coding for COVID-19 vaccine
- Medicare COVID-19 vaccine payment
Monoclonal antibodies and administrations currently authorized
For payment allowances and coding refer to the CMS vaccine pricing - COVID-19 vaccines and monoclonal antibodies and the CMS COVID-19 monoclonal antibodies webpages.
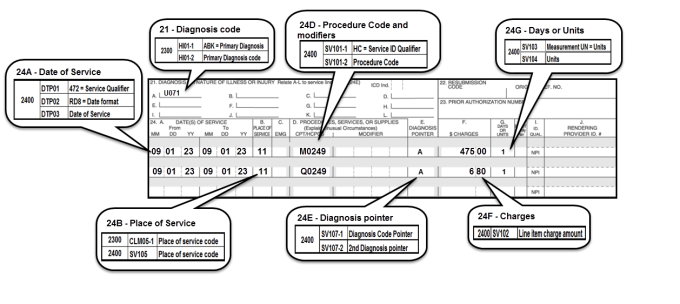
Claim submission example
- Claim should include the proper billing of the ICD-10 in item 21 or the EDI equivalent
- Use appropriate diagnosis coded to highest level of specificity:
- U071 - use as appropriate.
- Report the proper date of service
- Report the proper place of service
- Use the appropriate administration CPT or HCPCs code
- The diagnosis pointer should be used to indicate the primary diagnosis on the claim form
- Report the charge amount for each line item
References
- CDC COVID-19 vaccination clinical and professional resources
- COVID-19 frequently asked questions (FAQs) on Medicare fee-for-service (FFS) billing
- COVID-19 provider toolkit
- COVID-19 vaccines and monoclonal antibodies payment
- Medicare billing for COVID-19 vaccine shot administration
- Monoclonal antibody COVID-19 infusion
- SNF: Enforcement discretion relating to certain pharmacy billing
- Toolkit on COVID-19 vaccine: Health insurance and Medicare Advantage plans
- CMS IOM Pub. 100-02 Medicare Benefit Policy Manual, Chapter 15, Section 60
- CMS IOM Pub. 100-04 Medicare Claims Processing Manual, Chapter 18, Section 10