PC-ACE training module: Entering a claim
Claim entry: Medicare primary
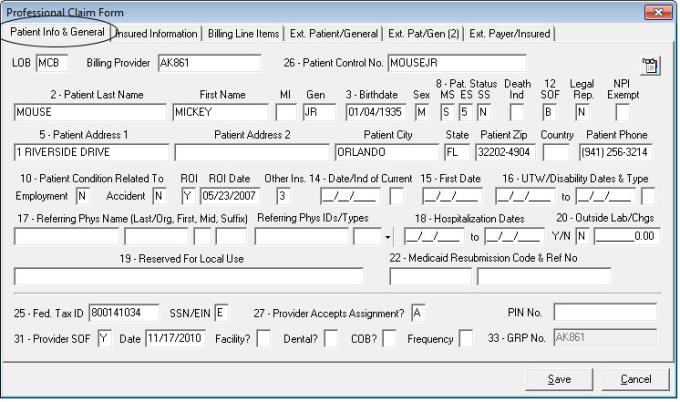
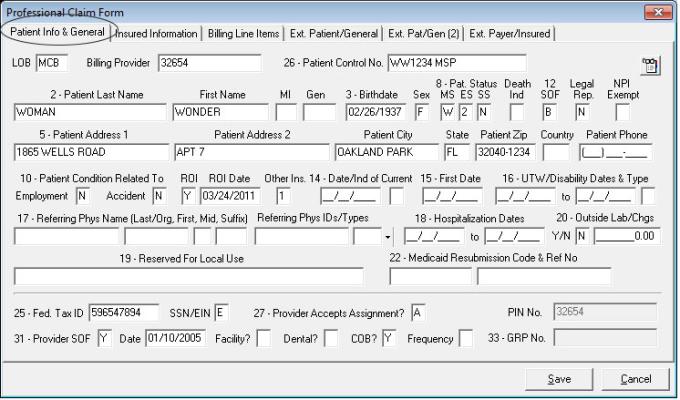
General
- Setup: Professional Claims Menu, Enter Claims, Patient Info & General
- Required: LOB, Billing Provider, Patient Control No, Employment, Accident, Outside Lab, Dental (for 837D claims only)
- Optional: Date/Ind of Current, First Date, UTW/Disability Dates & Types, Hospitalization Dates, Outside Lab Chgs, Facility, Referring Phys Name
- Leave blank: Medicaid Resubmission Code & Ref No, Dental (for 837 claims), COB, Frequency
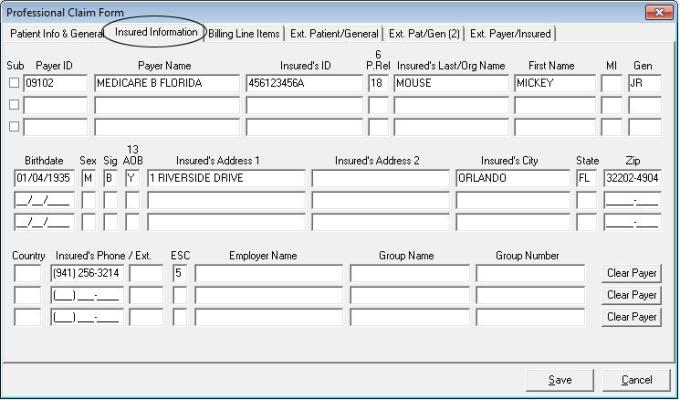
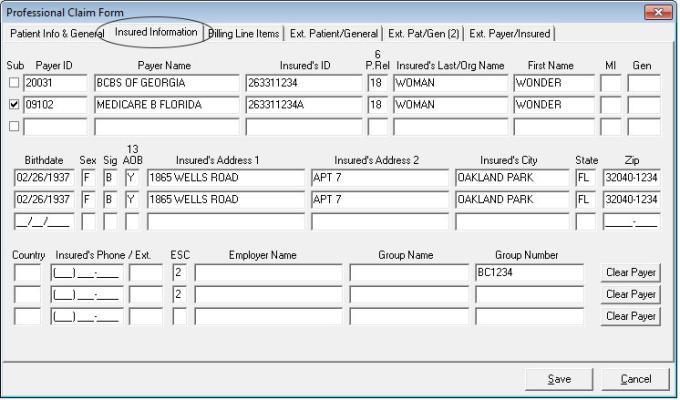
Insured information
- Setup: Professional Claims Menu, Enter Claims, Insured Information
- Information pulled from Patient database when patient selected on Patient Info & General Tab
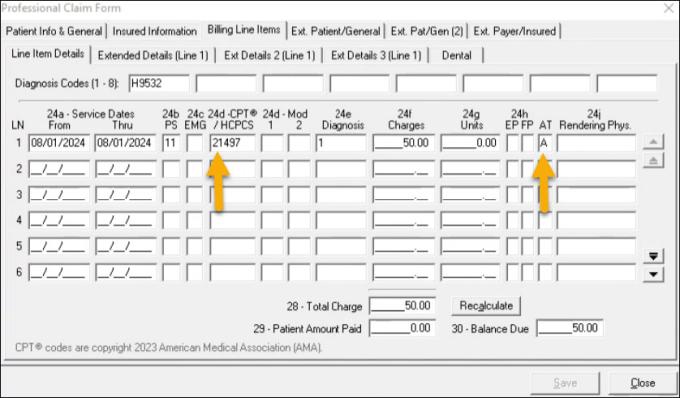
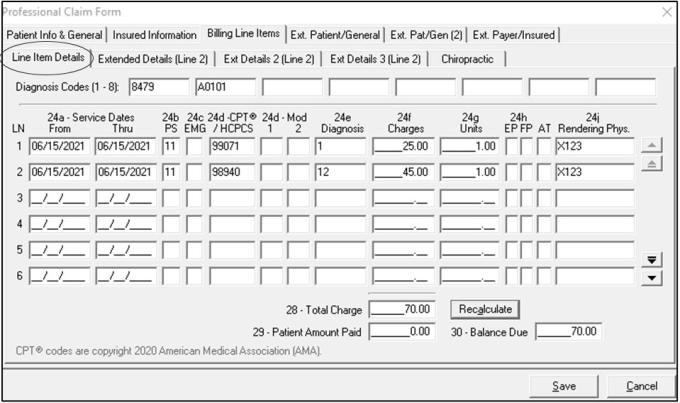
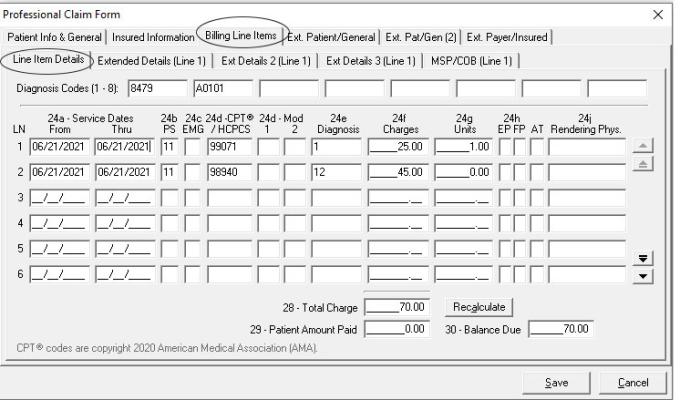
Line item details
- Setup: Professional Claims Menu, Enter Claims, Billing Line Items, Line Item Details
- Required: Diagnosis Codes (at least one), Service From/Thru Dates, Charges, PS, Proc, Diagnosis Pointer, Charges, Units, Rendering Phys. (unless billing as a Solo Provider), Total Charge, Dental tab (837D claims only)
- Optional: Additional Diagnosis, EMG, Modifiers, EP, FP, AT, Rendering Physician (unless billing as a group)
- Auto populated: Recalculate, Patient Amount Paid, and Balance due when Recalculate is selected
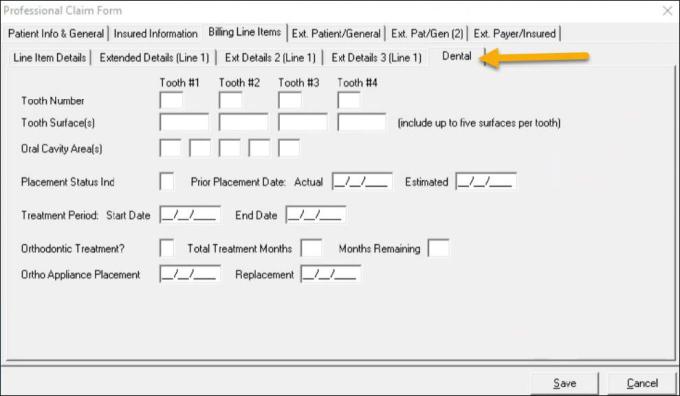
Line item details: Dental
- Setup: Professional Claims Menu, Enter Claims, Billing Line Items, Line Item Details
- The Dental tab will display when a valid dental HCPCS code is provided along with “A” in the 24h AT field
Tips
- Setup: Professional Claims Menu, Enter Claims, Billing Line Items, Line Item Details
- Tips: Right click or F2: Accesses information from databases or available pull down menus
F4: Field Duplication
F5: Line Duplication
F7: Line deletion
F8: Advance to next line
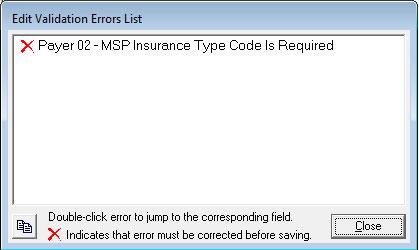
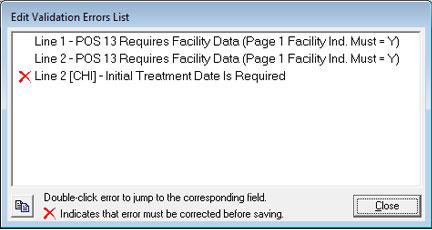
Edit validation errors list
Once “Save” is selected, the claim will edit for known requirements.
- Error message will indicate the line or field the error is associated with
- Double click on error to jump to corresponding field
- Once error is corrected select “Save” again to re-edit claim
- Red X error must be corrected before transmitting
- Only claims saved as CLN or ERR can be transmitted
Claim entry: Medicare secondary / payment made
General
- Setup: Professional Claims Menu, Enter Claims, Patient Info & General
- Required: LOB, Billing Provider, Patient Control No., Employment, Accident, Outside Lab, COB, Dental (for 837D claims)
- Optional: Date/Ind of Current, First Date, UTW/Disability Dates & Types, Hospitalization Dates, Outside Lab Chgs, Facility, Referring Phys Name
- Leave blank: Medicaid Resubmission Code & Ref No, Dental (for 837 claims), Frequency, Reserved For Local Use
Insured information
- Setup: Professional Claims Menu, Enter Claims, Insured Information
- Information pulled from Patient database when patient selected on Patient Info & General Tab
Line item details: MSP
- Setup: Professional Claims Menu, Enter Claims, Billing Line Items, Line Item Details
- Required: Diagnosis Codes (at least one), Service From/Thru Dates, PS, Proc, Diagnosis Pointer, Units, Rendering Phys (unless billing as a Solo Provider), Recalculate
- Optional: Additional Diagnosis, EMG, Modifiers, EP, FP, AT, Rendering Physician (unless billing as a group)
- Auto populated: Total Charge, Patient Amount Paid, and Balance due when Recalculate is selected
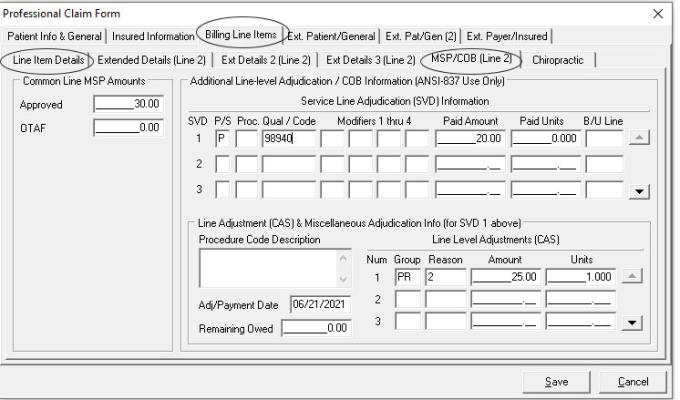
Line item details: MSP/COB line 1
- Setup: Professional Claims Menu, Billing Line Items, MSP/COB Line 1
- Required: Approved, SVD, CAS, Adj/Payment Date
- Leave blank: OTAF, Information on lines 2 and 3 of SVD and CAS, Procedure Code Description, Remaining Owed
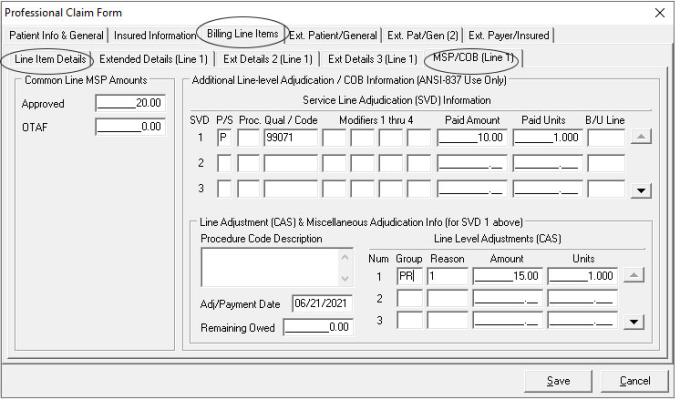
Line item details: MSP/COB line 2
- Setup: Professional Claims Menu, Billing Line Items, MSP/COB Line 2
- Required: Approved, SVD, CAS, Adj/Payment Date
- Leave blank: OTAF, Information on lines 2 and 3 of SVD and CAS Procedure Code Description, Remaining Owed
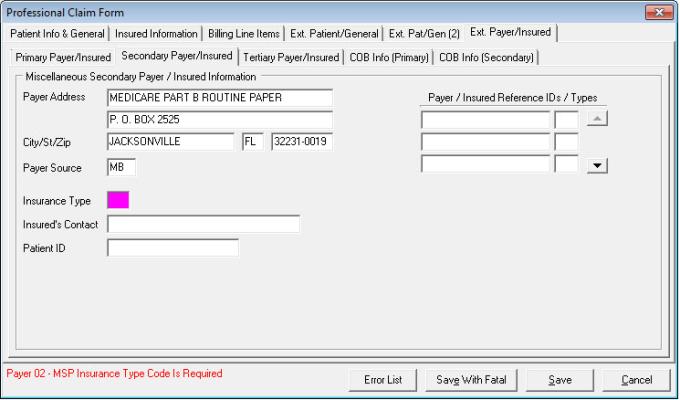
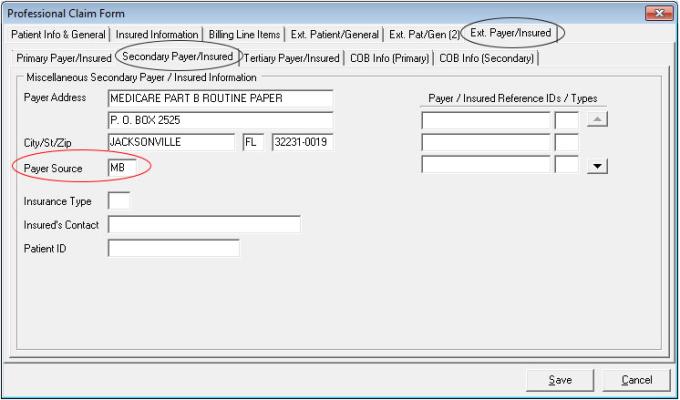
Ext payer insured: Secondary payer
- Setup: Professional Claims Menu, Ext. Payer/Insured, Primary Payer Insured
- Required: Insurance Type (insurance type was left blank for training purposes)
- Auto populates: Payer Address, Payer Source
- Optional: Insured’s Contact, Patient ID
- Leave blank: Payer/ Insured Reference IDs/Types
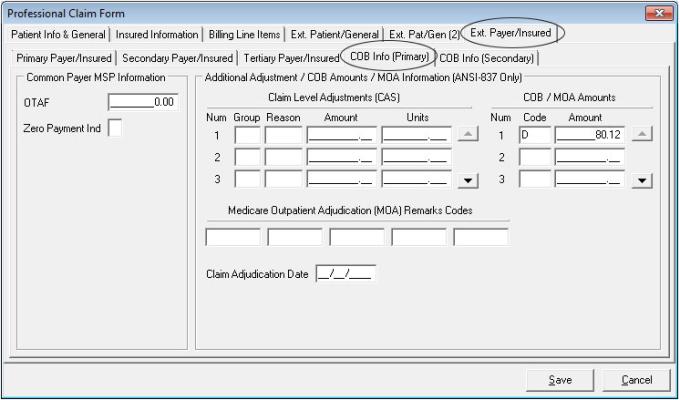
Ext payer insured: Secondary payer / COB info primary
- Setup: Professional Claims Menu, Enter Claims, Ext. Payer/Insured, COB Info (Primary)
- Required: Zero Payment Made Ind N – to indicate payment was made, COB Code (D – to indicate total claim payer paid amount), MOA Amount
- Leave blank: OTAF, CAS, Medicare Outpatient Adjudication (MOA) Remarks Codes, Claim Adjudication Date
Edit validation errors list
Once “Save” is selected, the claim will edit for known requirements.
- Error message will indicate the line or field the error is associated with
- Double click on error to jump to corresponding field
- Once error is corrected select “Save” again to re-edit claim
- Red X error must be corrected before transmitting